Sleep Disorders
- Clinician-reviewed sleep disorder diagnostics
- Personalised treatment backed by data
- CPAP therapy supported by ongoing care
Obstructive Sleep Apnoea - What You Need to Know
What is Sleep Apnoea?
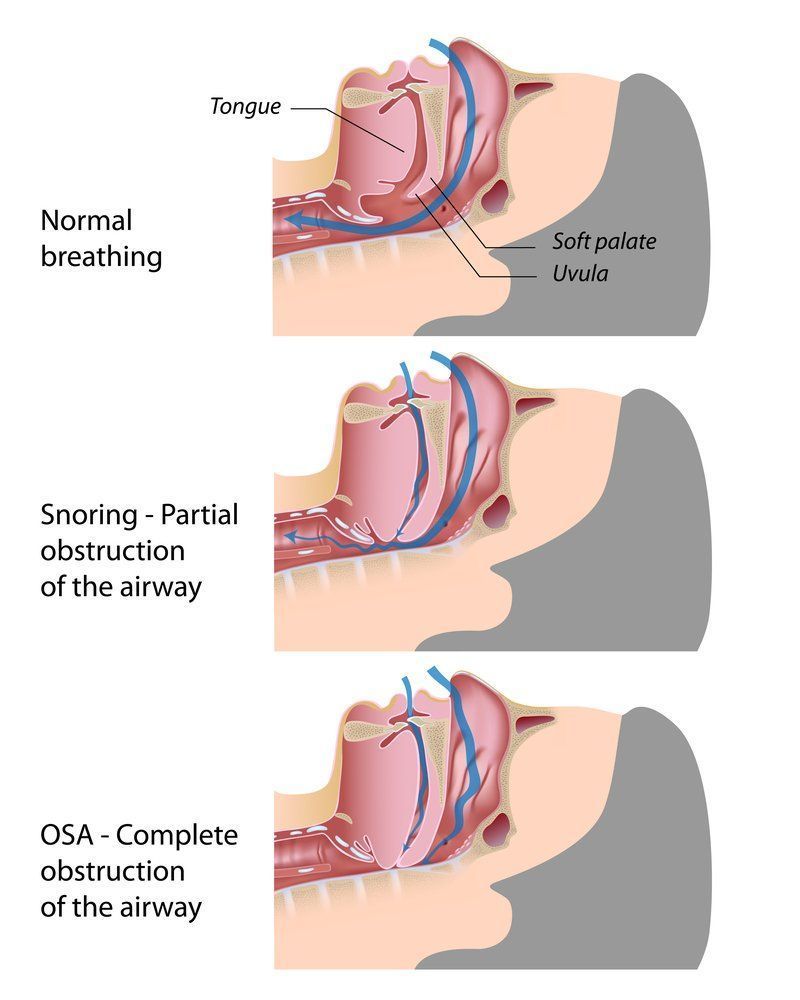
Sleep apnoea is more common than you might think - it affects about half of all men and nearly a quarter of women. The name comes from a Greek word meaning "without breath", which describes exactly what happens: you stop breathing multiple times during the night.
These breathing pauses last at least 10 seconds and can happen hundreds of times in a single night. Your oxygen levels drop, your brain wakes you up just enough to start breathing again, then you fall back asleep - often without even remembering it happened.
The main signs are:
- Persistent loud snoring
- Feeling tired during the day, no matter how much sleep you get
- Long pauses in breathing followed by gasping or choking sounds
Why This Matters to Your Health
When left untreated, moderate to severe sleep apnoea can increase your risk of high blood pressure, heart problems, heart attack and stroke by 5-10 times. It can also cause morning headaches, teeth grinding and problems with concentration and memory.
But here's the important part:
sleep apnoea can be diagnosed and successfully treated.
Who Gets Sleep Apnoea?
While it's more common in men, people who are overweight and older adults, we regularly see young, fit people with severe sleep apnoea too. It can affect anyone.
You're more likely to have sleep apnoea if you:
- Snore loudly and are overweight
- Have high blood pressure
- Have a thick neck or narrow airways
- Are over 40 (though younger people can have it too)
What Are the Effects?
During those breathing pauses, your oxygen drops and your brain has to wake you up to resume breathing. This constant interruption means you never get the deep, restorative sleep your body needs. This can lead to:
- Extreme daytime sleepiness
- Difficulty concentrating at work
- Mood changes and irritability
- Relationship problems
- Increased risk of car accidents (people with severe sleep apnoea are 2-3 times more likely to crash)
- Higher risk of heart problems and stroke
How Do We Diagnose Sleep Apnoea?
A sleep study is the only way to definitively diagnose sleep apnoea. Our home sleep studies are comprehensive and comfortable, recording your brain waves, muscle activity, heart rate, breathing patterns, oxygen levels and leg movements - all while you sleep in your own bed.
How is Sleep Apnoea Treated?
The good news is that sleep apnoea is very treatable. Treatment options include:
For Mild Cases:
- Weight loss (if overweight)
- Learning to sleep on your side instead of your back
- Avoiding alcohol and sleeping pills
- Quitting smoking
For Moderate to Severe Cases:
- CPAP therapy - This is the gold standard treatment. A comfortable mask delivers gentle air pressure to keep your airways open while you sleep.
- Oral appliances - Custom made devices that hold your jaw forward to keep airways open.
- Surgery - In some cases, procedures to remove obstructions or correct structural problems.
Can Sleep Apnoea be Prevented?
The best ways to reduce your risk are maintaining a healthy weight, sleeping on your side and avoiding alcohol before bed. Some people find that singing exercises can help strengthen throat muscles.
Snoring - More than Just a Nuisance
What Causes Snoring?
Snoring happens when airflow through your upper airway gets partially blocked. During sleep, all your muscles relax - including those in your throat and tongue. This can narrow your airway, causing the soft tissues to vibrate with each breath.
When is Snoring a Problem?
Besides keeping your partner (or neighbours!) awake, loud snoring can be a sign of sleep apnoea. If your snoring is interrupted by silent periods of 10-90 seconds, this could indicate sleep apnoea.
How We Can Help
Our sleep studies can measure exactly when and how loudly you snore. This is the only reliable way to determine if your snoring is linked to sleep apnoea, which helps us recommend the best treatment.
Treatment Options for Snoring:
- CPAP machines - Even without sleep apnoea, these can eliminate snoring
- Oral appliances - Custom made mouthguards that hold your jaw forward
- Mouth taping - Recent studies show this can reduce snoring in people who breathe through their mouth
- Positional therapy - Devices that help you stay sleeping on your side
- Lifestyle changes - Weight loss, avoiding alcohol before bed, treating nasal congestion
- Sleep position - Sleeping slightly elevated can help
Other Sleep Disorders We Can Help With
Insomnia
If you have trouble falling asleep, staying asleep or wake up too early, you might have insomnia. About 25% of insomnia cases are actually caused by physical problems like sleep apnoea or restless legs. Our sleep studies can help identify if there's a physical cause that can be treated.
Restless Legs Syndrome (RLS)
This involves uncomfortable sensations in your legs - described as creeping, crawling or tingling - along with an irresistible urge to move them. These symptoms are typically worse in the evening and can make it very difficult to fall asleep.
Periodic Limb Movements
This involves repetitive jerking or bending of the legs during sleep, often every 30 seconds. It can wake you up repeatedly throughout the night and leave you feeling exhausted the next day.
Narcolepsy
This rare disorder affects the brain's ability to control sleep-wake cycles. People with narcolepsy can fall asleep suddenly and without warning, even during activities like driving or working.
Don't Let Sleep Problems Control Your Life
Sleep disorders are real medical conditions that can seriously impact your health, relationships and quality of life. The good news is that most sleep disorders are very treatable once properly diagnosed.
If you're experiencing any of these symptoms, don't wait. The sooner we can identify what's disrupting your sleep, the sooner we can help you get back to sleeping well and feeling rested. Your first step is a conversation with your GP about whether a sleep study might be right for you.
Frequently Asked Questions
What are the most common types of sleep disorders?
There are more than 80 recognised sleep disorders, but the most common include obstructive sleep apnoea, insomnia, restless legs syndrome (RLS), narcolepsy, and circadian rhythm disorders. Obstructive sleep apnoea causes breathing to stop and start repeatedly during sleep, often due to airway collapse. Insomnia is characterised by difficulty falling asleep, staying asleep, or waking too early. RLS involves uncomfortable sensations in the legs, usually at night, leading to an irresistible urge to move them. Narcolepsy causes excessive daytime sleepiness and sudden sleep attacks, while circadian rhythm disorders disrupt the internal sleep-wake cycle, often due to shift work or irregular schedules. Each condition presents with different symptoms and requires specific diagnosis and treatment strategies.
What causes sleep disorders?
Sleep disorders can be caused by a variety of factors including medical conditions, lifestyle habits, psychological issues, and genetic predisposition. For example, obstructive sleep apnoea is often linked to physical factors such as enlarged tonsils, obesity, or a recessed jaw. Insomnia may be triggered by stress, anxiety, depression, or the use of stimulants like caffeine or certain medications. Restless legs syndrome is believed to have a neurological basis and may be hereditary or related to iron deficiency. Narcolepsy is thought to involve autoimmune responses affecting the brain's regulation of sleep. Environmental influences, irregular sleep schedules, and poor sleep hygiene can also contribute to the development or worsening of sleep disorders.
How do I know if I have a sleep disorder?
Common signs of a sleep disorder include loud snoring, gasping for air during sleep, frequent nighttime awakenings, difficulty falling or staying asleep, excessive daytime sleepiness, and trouble concentrating or remembering things. Some people also report mood changes, morning headaches, or a dry mouth upon waking. If these symptoms occur regularly and interfere with daily functioning, it’s a strong indication that a sleep disorder may be present. Diagnosis typically involves a clinical consultation and, in many cases, a sleep study to monitor breathing, heart rate, oxygen levels, and brain activity during sleep.